Dedicated to understanding how islet failure causes diabetes
Our lab focuses on the critical role of the islet in diabetes pathogenesis, and how novel aspects of the islet milieu contribute to failure of the islet β cell.
Our current research interests aims to answer three main questions:
1. How does the islet endothelial cell contribute to β cell failure in type 2 diabetes?
Islet endothelial cells develop an inflammatory and proadhesive phenotype in multiple models of diabetes. This is associated with altered compostion and remodeling of the islet extracellular matrix. Data from our lab and others suggest that both of these components contribute to decreased function and survival of the islet β cell. We are using novel in vitro approaches, along with animal models to understand how and why the islet endothelial cell becomes dysfunctional and how this affects β cell function in diabetes.
Current areas of interest are the roles of laminin (decreased production) and hyaluronan (increased production and fragmentation) in this process.
We are also generating human islet endothelial cells isolated from diabetic and non-diabetic donors for RNA-Seq, along with utilizing existing single cell RNA-Seq databases to better understand islet endothelial dysfunction in human diabetes.
2. What are the mechanisms underlying islet amyloid-mediated toxicity?
Our recent data suggest that islet endothelial cells are a novel target of islet amyloid toxicity, and islet amyloid-induced inflammation in islet endothelial cells has numerous downstream effects that impact the β cell. Specifically, these include further stimulation of islet amyloid formation, recruitment and activation of macrophages and direct effects to impair β cell function and/or survival. We are using cell-free systems, cultured islet endothelial cells and animal models to understand these new mechanisms of islet amyloid formation/toxicity.
3. What causes islet failure in cystic fibrosis-related diabetes?
Diabetes affects up to 50% of patients with cystic fibrosis, and abnormalities in insulin release are already present in very young children with the disease. Islet pathology and the mechanisms by which islet dysfunction occur in CFRD are still poorly understood. We recently found that islet inflammation is a widespread feature of CFRD, occurring even in young children with the disease; we are following up on those observations in the lab. Islet amyloid is also a common feature of CFRD, but it occurs decades earlier in this disease than it is typically seen in type 2 diabetes, suggesting a different etiology. We are studying a novel mouse model that expresses the most common human CF mutation along with amyloidogenic (human) islet amyloid polypeptide in order to better understand the role of islet amyloid in the development of CFRD.
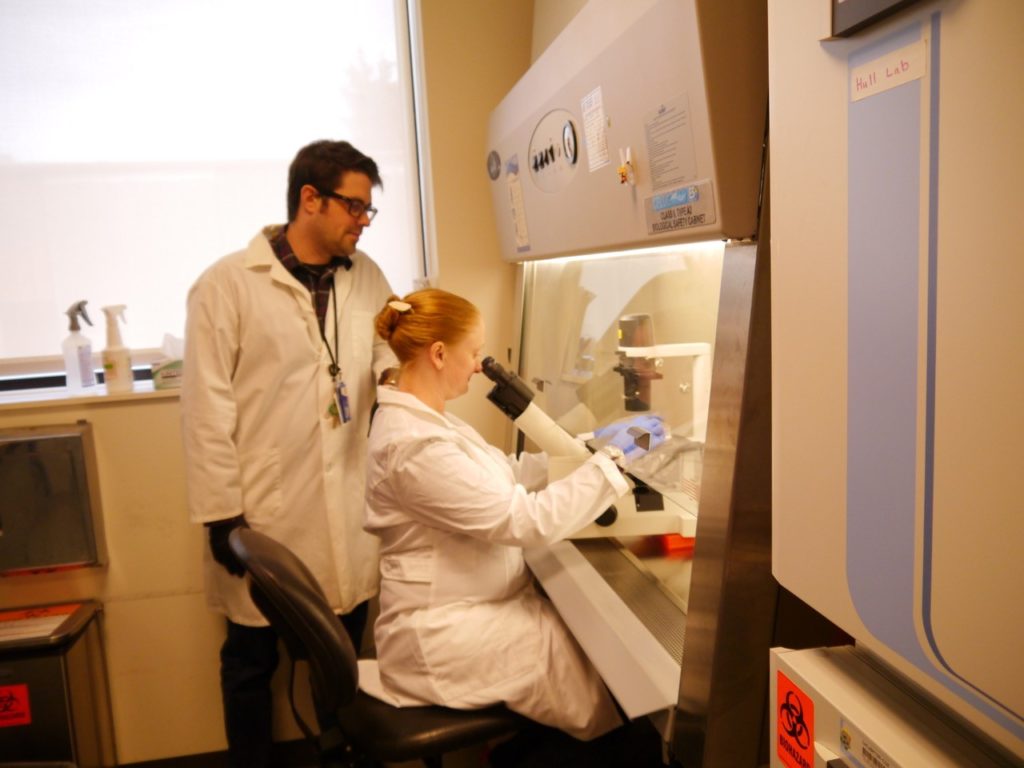
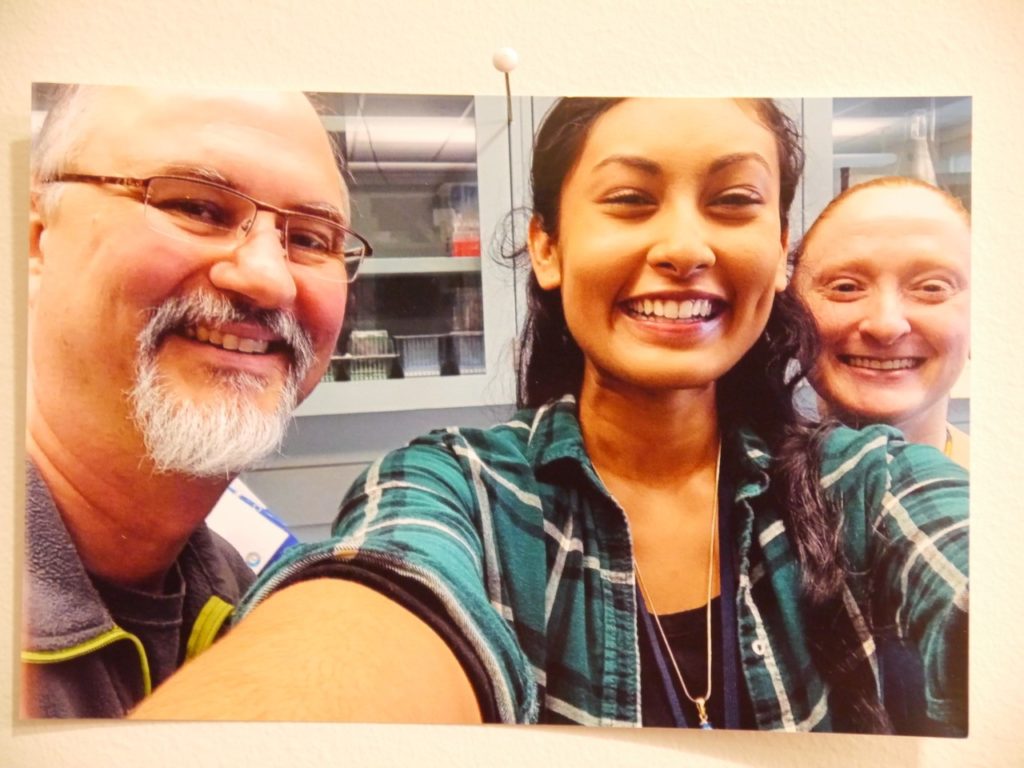
Lab Members

Rebecca Hull-Meichle, PhD
View Profile
Director, Diabetes and the Islet Program, UW Diabetes Institute
Research Professor of Medicine
Division of Metabolism, Endocrinology and Nutrition

Al Aplin, PhD

Daryl Hackney, BS

Meghan Hogan, PhD

Josh Castillo, PhD
Arianna Afshar
Lab Alumni
Jessica Kumar
Phil McNamara
Loren Hart
Zaheen Rabbani
Amy Liu
Len Tran
Contact Us
University of Washington
VA Puget Sound Health Care System
1660 S Columbian Way, Building 34, Room 228
Seattle, WA 98108
Phone/Fax: (206) 764-2897
Lab Phone: (206) 277-6795
Rebecca Hull-Meichle: rhull@uw.edu
Rebecca.Hull-Meichle@va.gov
To inquire about Postdoctoral and Graduate Student Openings click on: rhull.uw.edu